Brain Tumours
A brain tumour occurs when abnormal cells form within the brain. These can be malignant (cancerous) or benign (non-cancerous) and are classified as primary (originating in the brain) or secondary (spreading from other parts of the body).
Symptoms vary but often include headaches, seizures, vision problems, vomiting, and mental changes. The cause is usually unknown, though risk factors include exposure to ionising radiation, certain viruses, and inherited syndromes.
Signs and Symptoms
The signs and symptoms of brain tumours are broad and depend on the tumour's size, location, and growth rate. Common symptoms include headaches, which may worsen with Valsalva manoeuvre, cause awakening from sleep, and subside after vomiting. Location-specific symptoms vary:
- Frontal lobe: Poor reasoning, personality changes, poor planning, lower inhibition, and decreased speech production.
- Temporal lobe: Poor memory, hearing loss, and difficulty in language comprehension.
- Parietal lobe: Issues with language interpretation, speaking, writing, and spatial perception.
- Occipital lobe: Poor vision or loss of vision.
- Cerebellum: Poor balance, muscle movement, and posture.
- Brain stem: Seizures, endocrine problems, respiratory changes, visual changes, headaches, and partial paralysis.
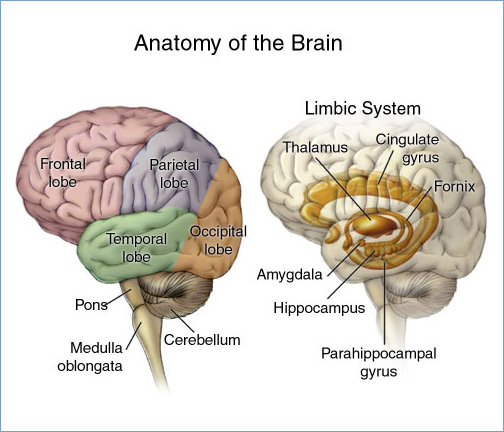
Personality and behavioural changes are also common, particularly with tumours affecting the frontal, temporal, and parietal lobes, leading to inappropriate social behaviour, temper tantrums, and psychological symptoms such as depression and anxiety.
Diagnosis
Diagnosis typically begins with a medical history and physical examination, followed by imaging techniques such as magnetic resonance imaging (MRI) and computed tomography (CT) scans.
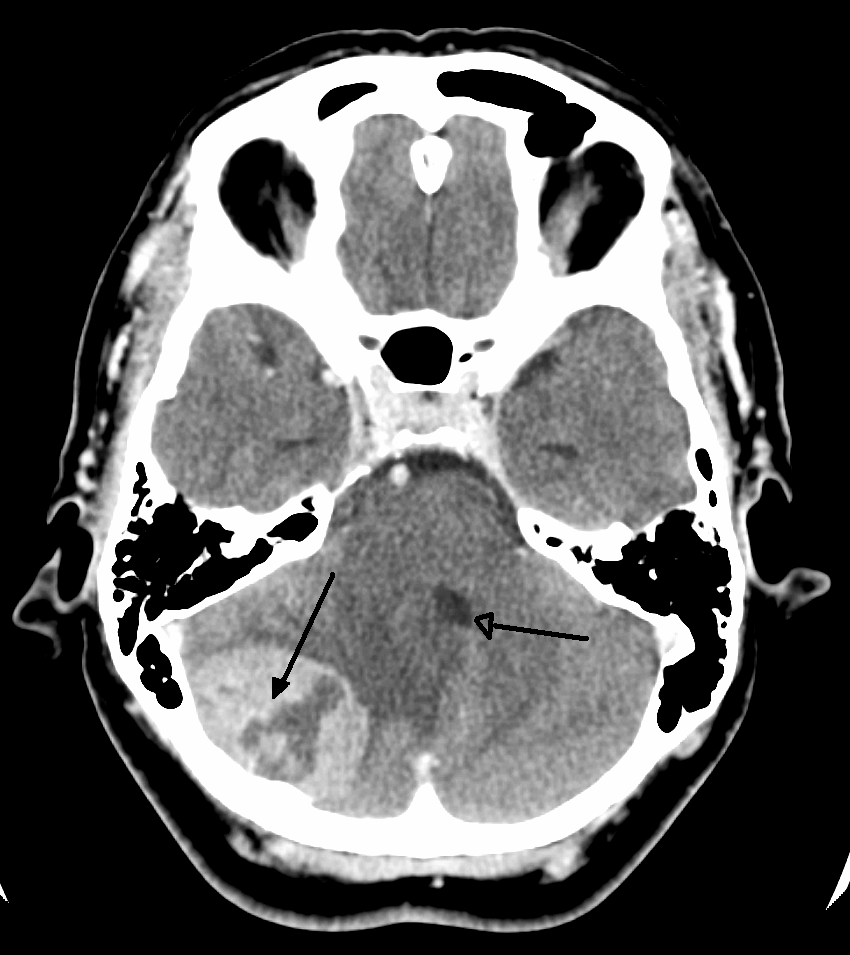
MRI is often the reference standard, though CT scans are used when MRI is contraindicated. Advanced MRI techniques like Magnetic Resonance Angiography (MRA), Magnetic Resonance Spectroscopy (MRS), Perfusion Magnetic Resonance Imaging (pMRI), Functional MRI (fMRI), and Diffusion Weighted Imaging (DWI) can provide additional physiological data. Positron Emission Tomography (PET) scans are also used, especially for high-grade tumours.

Histological examination of tumour tissue samples obtained via biopsy or surgery is essential for definitive diagnosis and treatment planning.
Treatment
Treatment options vary based on tumour type and location and may include surgery, radiation therapy, chemotherapy, or a combination of these.
Surgery
Surgical removal (resection) is the primary treatment, aiming for complete removal or maximal cytoreduction (debulking) of the tumour. Minimally invasive techniques are increasingly used. Postoperative radiotherapy and chemotherapy are standard for malignant tumours.
Radiation Therapy
Radiation therapy aims to kill tumour cells while sparing normal brain tissue. Techniques include external beam radiation and stereotactic radiosurgery. Whole-brain radiotherapy (WBRT) may be used for secondary brain tumours, while stereotactic radiotherapy is recommended for fewer, smaller secondary tumours.
Chemotherapy
Chemotherapy is used less frequently due to the blood-brain barrier but remains a treatment option, especially for malignant tumours. Its use is guided by the tumour's genetic mutations, which affect responsiveness.
Prognosis
Prognosis varies significantly based on tumour type, genetic mutations, and patient factors. Glioblastoma, the most aggressive primary brain tumour, has a median survival of 15 months with aggressive treatment. Oligodendrogliomas, though incurable, have a relatively better prognosis with a median survival of up to 16.7 years. Acoustic neuromas, being non-cancerous, can be managed effectively with surgery or radiation.

Epidemiology
Brain tumour incidence varies globally, with higher rates in developed countries. In the US, around 23,880 new cases were expected in 2018, with a median diagnosis age of 58 years. In the UK, brain tumours are the ninth most common cancer, with about 10,600 cases diagnosed annually.
Children
Brain tumours are the most common cancer in children under 19 and the leading cause of cancer death in this group. The most common types include pilocytic astrocytoma, malignant glioma, and medulloblastoma. The average survival rate for primary brain cancers in children is 74%.

Research
Research is ongoing in areas such as immunotherapy and the use of retroviral replicating vectors. Non-invasive detection methods using liquid biopsy are also being developed.
Self-assessment MCQs (single best answer)
What is the primary imaging technique used for diagnosing brain tumours?
Which lobe of the brain, when affected by a tumour, is most likely to cause poor balance and muscle movement issues?
Which of the following is NOT a common symptom of a brain tumour?
Which type of brain tumour is known to have the most aggressive prognosis?
What is the main goal of surgical treatment for brain tumours?
Which imaging technique is used specifically to provide physiological data about brain tumours?
What is the approximate median survival for patients with glioblastoma receiving aggressive treatment?
Which factor is NOT considered a risk factor for developing a brain tumour?
Which brain tumour type is most common in children under 19 years of age?
Which of the following advanced MRI techniques is used to measure brain activity by detecting changes associated with blood flow?
Dentaljuce
Dentaljuce provides Enhanced Continuing Professional Development (CPD) with GDC-approved Certificates for dental professionals worldwide.
Founded in 2009 by the award-winning Masters team from the School of Dentistry at the University of Birmingham, Dentaljuce has established itself as the leading platform for online CPD.
With over 100 high-quality online courses available for a single annual membership fee, Dentaljuce offers comprehensive e-learning designed for busy dental professionals.
The courses cover a complete range of topics, from clinical skills to patient communication, and are suitable for dentists, nurses, hygienists, therapists, students, and practice managers.
Dentaljuce features Dr. Aiden, a dentally trained AI-powered personal tutor available 24/7 to assist with queries and provide guidance through complex topics, enhancing the learning experience.
Check out our range of courses, or sign up now!