Antibiotic prescribing
Dento-alveolar infections

“Dento-alveolar” includes apical and periodontal abscesses and infections.
Chronic infections
Chronic apical abscesses (usually from pulp death), and periodontal abscesses, are usually well localised and not particularly painful. They may become acute (a “flare-up”) which can be very painful due to the pressure of trapped pus, or they may form a sinus that allows the pus to drain and give little trouble apart from a bad taste.
When do you need antibiotics for chronic dento-alveolar infections?
Local measures for treatment of chronic dento-alveolar infections.
Extracting a tooth provides a path for pus to escape – that is, extraction enables drainage. Usually no more treatment is needed.
If not extracting, abscesses need to be provided with a path to drain. There may already be a sinus, but if not, a path can be created by incising the abscess with a scalpel or a wide needle.
With periodontal abscesses, the infected pocket causing the abscess should be thoroughly debrided using ultrasonic and hand instruments. This will normally allow the pus to drain up the pocket into the mouth.
Sometimes one cannot achieve the necessary anaesthesia for immediate debridement (it is not good practice to inject LA into an abscess). Here, the abscess should be incised for drainage, then debridement with LA arranged soon afterwards.
For apical abscesses, it is usually bacteria within the root canal system that “feed” the abscess, and good quality root canal therapy will remove this cause, allowing healing.
If you open a tooth to allow drainage through the canal, ideally, the drainage will be supervised in the treatment room under rubber dam with regular irrigation. One should not leave teeth on unsupervised “open drainage” Click here
https://onlinelibrary.wiley.com/doi/full/10.1046/j.1365-2591.2001.00396.x
Particles of food material of vegetable origin (containing cellulose) may also be inadvertently pushed into the periradicular tissues of teeth … that have been left open for drainage ... In addition, … food may also carry microorganisms into the root canal system and/or the periradicular tissues. The practice of leaving a tooth open to drainage has been considered as unscientific for many years (Walker 1936). Complications rarely occur if clinical practice is based on the contemporary biological principles of endodontics. In contrast, complications arising from a tooth that has been left open to drain are usually difficult to treat (Weine et al. 1975).
It used to be thought that if antibiotics were given after endodontic treatment, it would be more successful. It has now been proved untrue. In clinical trials, patients had just as much pain, just as much swelling, and took just as many painkillers irrespective of whether they were on antibiotics or not.
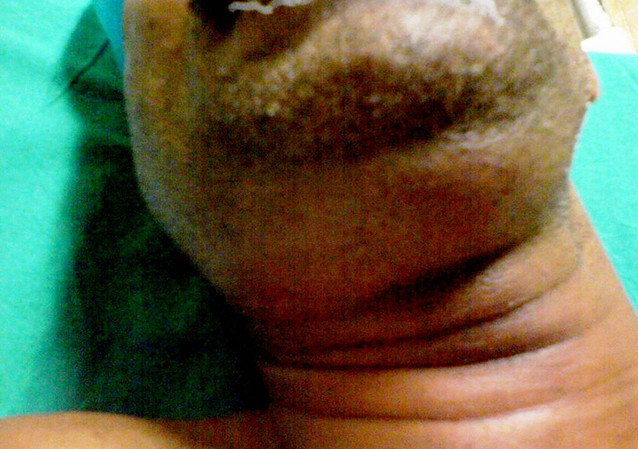
Acute dento-alveolar infections.
If these spread, they can have serious consequences, particularly for child patients or people who are immunocompromised.
When do you need antibiotics for acute dento-alveolar infections.?
When would you immediately refer the patient to a hospital or secondary care centre instead of treating them yourself?
How long should the patient take antibiotics?
How does resistance come about?
Click here
The body is full of bacteria, most of them are either helpful or at least harmless. These ones are called commensals. Pathogenic bugs have to compete with these “good” bacteria for living space, and usually do badly – which is why we are rarely ill.
Antibiotics however kill many of the good bacteria as easily as the pathogenic bacteria. After a long course of antibiotics, when resistant bugs have developed, the susceptible bacteria have effectively been wiped out and the resistant bugs can colonise the new "empty" places in the body. The pathogens do better than expected because they are not competing for space with commensals.
Over time, the “old bacteria” species (commensals) will return, but the resistant ones already present can trade genes with them, turning them also into resistant bacteria. These newly resistant commensals can then trade genes with new pathogenic bacteria, making them resistant too.
So you can end up with a body-full of resistant organisms, both good and bad, when it all started with just a few resistant pathogens left behind after the antibiotics.
Bad news if you need antibiotics again in the future…
As well as reducing the prevalence of resistant organisms, a short course also reduces the chance of side effects, allergic reactions, or sensitising people.
However, excess unused antibiotics in packets from courses that are stopped short tend to be flushed away by patients and end up in the water table, with environmental consequences. Explain to the patient they must not go in the bin, down the sink or the toilet. They must be taken to a pharmacy for safe disposal.
Recommended doses for dento-alveolar infections:
Adults and over-6s: 500mg three times a day, for up to 5 days.
1-5 years: 250mg three times a day, for up to 5 days.
Less than 1 year: 125mg three times a day, for up to 5 days.
Review at 2-3 days, and stop if resolved.
Use metronidazole when the patient is allergic to penicillin.
Use it together with Amoxicillin if the infection is severe and spreading (in non-allergic patients).
Adults and over-10s: 400mg three times a day, for up to 5 days.
7-10 years: 200mg three times a day, for up to 5 days.
3-7 years: 200mg two times a day, for up to 5 days.
1-3 years: 100mg three times a day, for up to 5 days.
Review at 2-3 days, and stop if resolved.
If neither of these are suitable, you can use Azithromycin or Clarithromycin as a third choice.
You should not use powerful “last resort” drugs like Co-Amoxiclav or Clindamycin. They don’t work any better, and can lead to resistance.