Antibiotic prescribing
Dry socket (alveolar osteitis)
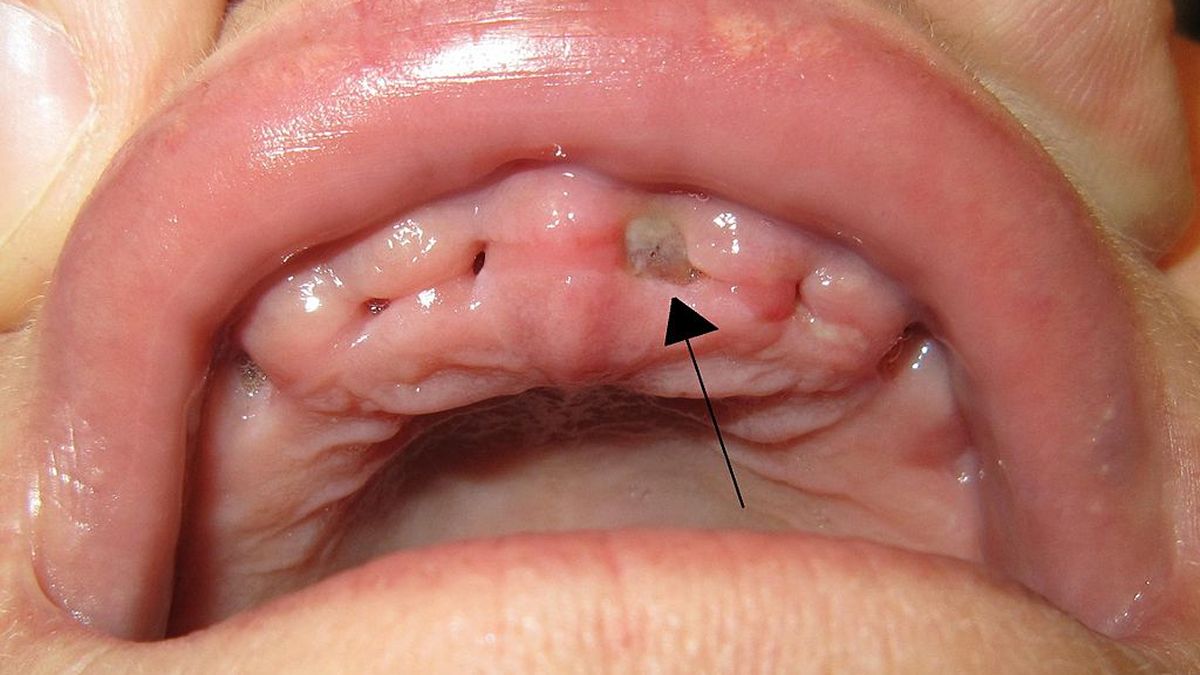
Dry socket upper left central incisor. Note absence of blood clot in socket, and exposed alveolar bone.
Alveolar osteitis, also known as dry socket, is inflammation of the alveolar bone of the maxilla or mandible. Classically, this occurs as a postoperative complication of tooth extraction.
A dry socket usually occurs where the blood clot fails to form or is lost from the socket. This leaves an empty socket where bone is exposed to the oral cavity, causing a localised alveolar osteitis limited to the lamina dura (the compact bone which lines the socket). It is associated with increased pain and delayed healing time.
Dry socket occurs after about 0.5–5% of all routine dental extractions.
How often does it occur after extractions of impacted mandibular third molars?
How many days after an extraction does it usually occur, and how long does it last?
A dry socket forms when the blood clot that should fill the socket is lost, or doesn't form. The socket bone (lamina dura) is exposed, and the marrow (in the medullary spaces) under it gets inflamed. The bone then becomes necrotic, and these dead areas are separated off by osteoclasts to form sequestrae. Note this is the result of inflammation of the marrow, not infection by bacteria.
How should a dry socket be treated?
Bacteria may enter the dry socket and cause a secondary infection. Also, a socket may get infected by bacteria without going through the "dry socket" stage.
If there is evidence of systemic spread of such a secondary infection, antibiotics may be prescribed (Amoxicillin or Metronidazole). They should not be prescribed if the infection is localised.